Sports Injuries,Acute Injuries And Overuse Injuries:
Regular physical activity is probably the most important overall determinant of a population’s health. Unfortunately, physical activity may extract a cost in the form of an activity-related injury. Such an injury may be categorised as either being an acute injury or an overuse injury depending on the mechanism of injury and the onset of symptoms.
Acute Injuries
Acute injuries may be due to extrinsic causes, such as a direct blow, either as a result of contact with another player or equipment, or intrinsic causes, such as a ligament sprain or muscle tear. Acute injuries may be classified according to the particular site injured (e.g. bone, cartilage, joint,ligament, muscle, tendon, bursa, nerve or skin) and the type of injury (e.g. fracture, dislocation, sprain or strain).
Overuse Injuries
Overuse injuries present three distinct challenges to the clinician-diagnosis, treatment and an understanding of why the injury occurred. Diagnosis requires taking a comprehensive history of the onset, nature and site of the pain along with a thorough assessment of potential risk factors, for example, training and technique. Careful examination may reveal which anatomical structure is affected. It is often helpful to ask patients to perform the maneuver that produces their pain.
Causes of Overuse Injuries
A cause must be sought for every overuse injury. The cause may be quite evident,
- Such as a sudden doubling of training quantity,
- Poor footwear or an obvious biomechanical abnormality or may be more subtle, such as running on a cambered surface, muscle imbalance or leg length discrepancy.
- The causes of overuse injuries are usually divided into extrinsic factors such as training, surfaces, shoes, equipment and environmental conditions.
- Intrinsic factors such as malalignment, leg length discrepancy, muscle imbalance, muscle weakness, lack of flexibility and body composition.
- Possible factors in the development of overuse injuries.
Treatment of Overuse Injuries
The treatment of overuse injuries may include relative rest, that is,
- Avoidance of aggravating activities
- While maintaining fitness
- The use of ice and various electrotherapeutic modalities
- Soft tissue techniques; and drugs
- Such as the non-steroidal anti-inflammatory drugs (NSAIDs).
Bone
Stress fractures
Stress fractures, a common injury among sportspeople, were first reported in military recruits in the l9th century. A stress fracture is a micro fracture in bone that results from repetitive physical loading below the single cycle failure threshold. Overload stress can be applied to bone through two mechanisms:
- The redistribution of impact forces resulting in increased stress at focal points in bone.
- The action of muscle pulls across bone.
Histological changes resulting from bone stress occur along a continuum beginning with vascular congestion and thrombosis. This is followed by osteoclastic and osteoblastic activity leading to rarefaction, weakened trabeculae and micro fracture and ending in complete fracture. This sequence of events can be interrupted at any point in the continuum if the process is recognized.
Similarly, the process of bony remodeling and stress fracture in athletes is recognized as occurring along clinical continuum with pain or radiographic changes presenting identifiable markers along the continuum. Since radioisotopic imaging and MRI can detect changes in bone at the phase of accelerated remodeling, these investigations can show stress-induced bony changes early in the continuum.
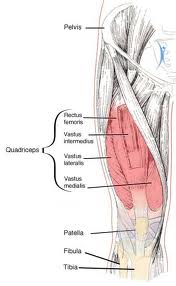
Stress fractures may occur in virtually any bone in the body. The most commonly affected bones are the tibia, metatarsals, fibula, tarsal navicular, femur and pelvis. A list of sites of stress fractures and the likely associated sports or activities.
It is important to note that a bone scan, although a routine investigation for stress fractures, is non-specific, and other bony abnormalities such as tumors and osteomyelitis may cause similar pictures. It may also be difficult to localize the site of the area of increased uptake precisely,especially in an area such as the foot where numerous small bones are in close proximity.
Diagnostic Features of A Stress Fracture
- Localized pain and tenderness over the fracture site.
- A recent change in training or taking up a new activity.
- X-Ray appearance is often normal or there may be a periosteal reaction.
- Abnormal appearance on radioisotopic bone scan scintingraphy), CT scan or MRI.
MRI is being increasingly advocated as the investigation of choice for stress fractures. Even though MRI does not image fractures as clearly as do computed tomography (CT) scans, it is of comparable sensitivity to radioistopic bone scans in assessing bony damage. The typical MRI appearance of a stress fracture shows periosteal and marrow edema plus or minus the actual fracture line.
Treatment of Stress Fractures
The treatment of stress fractures generally requires avoidance of the precipitating activity.
- The majority of stress fractures heal within six weeks of beginning relative rest.
- Healing is assessed clinically by the absence of local tenderness and functionally by the ability to perform the precipitating activity without pain.
- It is not useful to attempt to monitor healing with X-ray or radioisotopic bone scan.
- CT scan appearances of healing stress fractures can be deceptive as in some cases the fracture is still visible well after clinical healing has occurred.
- The return to sport after clinical healing of a stress fracture should be a gradual process to enable the bone to adapt to an increased load.
- An essential component of the management of an overuse injury is identification and modification of risk factors.
- There are, however, a number of sites of stress fractures in which delayed union or non-union of the fracture commonly occurs.
- These fractures need to be treated more aggressively.
- The sites of these fractures and the recommended treatments.
Bone Strain
In some athletes bone scans show uptake of radioisotope at non-painful sites. This is thought to represent bony remodeling at a very early subclinical level and has been termed ‘bone strain‘. Another situation encountered in clinical practice is the painful tender focal area of bone that demonstrates a mildly increased uptake of radioisotope on bone, insufficient to be classified as a stress fracture. This has been termed ‘stress reaction’. It would appear that there is a continuum of bone response to stress that ranges from mild (bone strain) to severe (stress fracture). The clinical features of bone strain, stress reaction and stress fractures.
The presence of bone strain or a stress reaction are probably an indication that the patient is moving further along the continuum towards a stress fracture and should probably be an indication for reduction or modification of activity.
Articular cartilage
Overuse injury can affect the articular cartilage lining of joints, particularly in osteoarthritis. Changes range from microscopic inflammatory changes to softening, fibrillation, fissuring and ultimately to gross visible changes. In younger people, this pathology can arise at the patella (patellofemoral syndrome), but it is important to note that the pain of patellofemoral syndrome can occur in the presence of normal joint surfaces.
Joint
Inflammatory changes in joints associated with over use are classified as synovitis or capsulitis. Examples of these problems are the sinus tarsi syndrome of the subtalar joint and synovitis of the hip joint.
Ligament
Overuse injuries of ligaments are uncommon. The medial collateral ligament of the knee occasionally becomes inflamed, particularly in breaststroke swimmers.
Muscle
Focal tissue thickening/fibrosis
Repetitive microtrauma caused by overuse damages muscle fibers. This is thought by some to lead to development of adhesions between muscle fibers and formation of cross-linkages in fascia.
Clinically, these changes may be palpated as firm focal areas of tissue thickening, taut, thickened bands arranged in the direction of the stress or as large areas of increased muscle tone and thickening.
These lesions may cause local pain or predispose other structures, such as tendons, to injury due to reduction in the ability of the tissue to elongate under stretch or eccentric load. This will also compromise the ability of the affected muscle to contract an relax rapidly.
These minor muscle injuries, which occur frequently in association with hard training, may respond to regular soft tissue therapy, strengthening and stretching.
Tendon
Tendon injuries are among the most common overuse injuries. Tendons, which are made up of tight parallel collagen bundles, transmit forces from muscle to bone and are, therefore, subject to great tensile stresses. Tendons withstand strong tensile forces, resist shear forces less well and provide little resistance to compression force. The stress-strain curve for tendons. As the strain increases, tissue deformation begins, some fibers begin to fall and ultimately macroscopic tendon failure occurs. There is, however, a large margin between the stresses that cause tendon failure and those that are experienced during normal physiological loading.
The vasculature of tendons is variable with the blood supply originating at both the musculotendinons and bone-tendon junctions. Vascular tendons are surrounded by a paratenon and avascular tendons are in sheaths. Tendon vascularity is compromised at site of friction, torsion or compression.
Bursa
The body contains many bursae situated usually between bony surfaces and overlying tendons. Their role is to facilitate movement of the tendon over the bony surface. Overuse injuries in bursae are quite common, particularly at the subacromial bursa, the greater trochanteric bursa, the bursa deep to the iliotibial band at the knee and the retrocalcaneal bursa separating the Achilles tendon from the calcaneus.
Bursitis is associated with local tenderness and swelling and pain on specific movements. Treatment involves the use of NSAIDs but this may be ineffective due to the poor blood supply of most bursae. Occasionally, a bursa needs to be drained of its fluid with or without subsequent corticosteroid infiltration.
Nerve
Nerve entrapment syndromes occur in athletes as a result of swelling in the surrounding soft tissues or anatomical abnormalities. These may affect the suprascapular nerve, the posterior interosseous, ulnar and median nerves in the forearm, the obturator nerve in the groin, the posterior tibial nerve at the tarsal tunnel on the medial aspect of the ankle and, most commonly, the interdigital nerves, especially between the third and fourth toes, a condition known as a Morton’s neuroma. This condition is not a true neuroma but rather a nerve compression. These nerve entrapments occasionally require surgical decompression.
Chronic Mild irritation of a nerve may result in damage manifested by an increase in neural tension. These may be the primary cause of the patient’s symptoms or may contribute to symptoms.
Skin
Blisters may occur at any site of friction with an external source or sporting equipment. Foot blisters can be prevented by wearing-in new shoes, wearing socks , and smearing petroleum jelly over the sock at sites of friction .Strategies to prevent blisters also serve to prevent callus. symptomistic callus can be pared down with a scalpel blade, taking care not to lacerate the normal skin.
At the first sign of a blister, the aggravating source should be removed and either adhesive tape applied over the blistered area or blister pads should be applied. Blister pads prevent blisters by acting as a barrier between skin and shoe. Treatment of blisters involves prevention of infection by the use of antiseptics and protection with sticking plaster. Fluid-filled blisters may be punctured and drained.
Clinical Presentation of Patient’s with Overuse Pain
- Pain some time after exercise or, more frequently, the following morning upon rising.
- Can be painful at rest and initially becomes less painful with use.
- Athletes can run through the pain or the pain disappears when they warm up, only to return after exercise when they cool down.
- The athlete is able to continue to train fully in the early stages of the condition; this may interfere with the healing process.
- Examination, local tenderness and thickening.
- Frank swelling and crepitus may be present, although crepitus is more usually a sign of associated tenosynovitis or is due to the hydrophilic (water attracting)nature of the collagen disarray (it is not ‘inflammatory fluid’).