Treatment of Knee Pain:
Definition of Patellofemoral Pain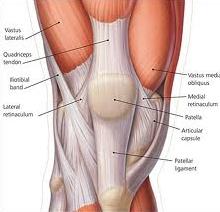
Patellofemoral pain is the preferred term used to describe pain in and around the patella. Synonyms include PFJ syndrome, anterior knee pain and chondromalacia patellae.
Patellofemoral pain is an umbrella term used to embrace all peripatellar or retro patellar pain in the absence of other pathologies. Since the cause of the pain may differ between patients, it is appropriate to review the potential sources of patellofemoral pain. A number of extra- and intra-articular components of the knee can generate neurosensory signals that ultimately result in of the patient feeling pain. Patellofemoral articular cartilage cannot directly be a source of pain.
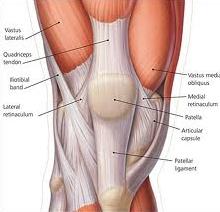
Functional Anatomy
- At full extension, the patella sits lateral to the trochlea.
- During flexion, the patella moves medially and comes to lie within the Intercondylar notch until 130 degree of flexion, when it starts to move laterally again.
- The patell mediolateral excursion is controlled by the quadriceps muscles, particularly the VMO and vastus lateralis components.
- With increasing knee flexion, a greater area of patellar articular surface comes into contact with the femur, thus offsetting the increased load that occurs with flexion.
- Loaded knee flexion activities subject the PFJ to loads many times the body weight, ranging from 0.5 times body weight for level walking to seven to eight time’s body weight for stair climbing.
Factors That May Contribute To Development of Pain
- Remote Contributing Factors
- Local Contributing Factors
Increased PFJ load instigates the development of patellofemoral pain. Factors that influence PFJ load can be considered in two categories: extrinsic and intrinsic.
- During physical activities the extrinsic load is created by the body’s contact with the ground (ground reaction force) and is therefore moderated by body mass, speed of gait, surfaces and footwear.
- During weight-bearing activities, any increase in the amount of knee flexion will increase the PFJ load.
- Intrinsic factors can influence both the magnitude and the distribution of the PFJ load.
- Distribution of load is conceptualized as movement of the patella within the femoral trochlea: patella tracking.
- Local factors that influence patella movement include patella position, soft tissue tension and neuromuscular control of the medial and lateral components of the vasti.
- The clinician should assess the contribution of various extrinsic and intrinsic factors to the development of patellofemoral pain.
- This assessment is crucial in the planning of an appropriate treatment regimen.
- The history will elucidate valuable information pertaining to extrinsic factors but clinical examination is usually required to evaluate most intrinsic contributing remote and local factors.
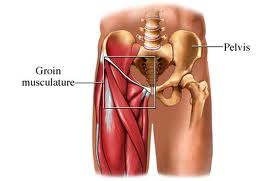
1. Remote Contributing Factors
The following remote factors may contribute to the development of patellofemoral pain:
- Increased femoral internal rotation
- Increased knee valgus
- Increased tibial rotation
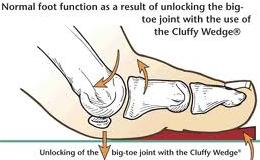
- Increased subtalar pronation
- Inadequate flexibility
It is important to assess the patient in static postures as well as functional activities. Some factors may become more obvious during specific functional tasks, such as the step-down or single-leg squat, where the postural demands are high.
2. Local Contributing Factors
Local factors that can contribute to the development of patellofemoral pain are:
- Patella position
- Soft tissue contributions
- Neuromuscular control of the vasti
Treatment of Patellofemoral Pain
The management of a patient with patellofemoral pain requires an integrated approach that may include:
- Reduction of pain and inflammation
- Addressing extrinsic contributing factors
- Addressing intrinsic contributing factors:
- Evidence base for physical intervenons
- Surgery-to be avoided
Immediate Reduction of Pain
The first priority of treatment is to reduce pain. This may require some or all of the following: rest from aggravating activities, ice, a short course of NSAIDs, electrotherapeutic modalities (e.g. ultrasound) and techniques such as mobilization or dry needling or acupuncture. Taping should have an immediate pain-relieving effect.
Addressing Extrinsic Contributing Factors
While initially it is vital to advise the patient to reduce the load on the PFJ, as rehabilitation progresses it is essential that any extrinsic factors that may have been placing excessive load on the PFJ (e.g. training, shoes and surfaces) are discussed and modified if necessary.
Addressing Intrinsic Contributing Factors
The clinician should have ascertained from the outset whether any intrinsic factors may have contributed to the development of the patient’s pain. Remote intrinsic factors may be addressed through hip muscle retraining, improving musculotendinous compliance or foot orthoses. Local intrinsic factors may be addressed with techniques such as patella taping or bracing, improving lateral soft tissue compliance, generalized quadriceps strengthening or vasti retraining.
Evidence Base for Physical Intervenons
A number of controlled clinical trials have assessed the effectiveness or efficacy of physical interventions for patellofemoral pain. While these reflect some aspects of treatment techniques, mostly the interventions are not individualized to the patients needs.
Treatment options that have gained popularity more recently have not been evaluated as thoroughly. The level 1 (systematic reviews) and level 2 (controlled clinical trials) evidence of the evaluation of physical interventions for patellofemoral pain.
Surgery-To Be Avoided
Experienced clinicians will have observed that the need for surgery in patellofemoral pain has been greatly reduced. This is likely due to the availability of evidence-based, exercise-based, physical interventions. To our knowledge, there has been no surgical randomized controlled trial showing the effectiveness of treatments such as chondroplasty or lateral release for patellofemoral pain. Thus, at a time when systematic reviews (level evidence) argue for physical therapies for this condition, it would appear that such avenues should be tried repeatedly and with various expert physical therapists before being abandoned in favor of a hoped-for surgical miracle. We note that poor surgical outcomes have been reported and often patellofemoral pain is worsened after surgery.
Active Physical Therapy’s experienced dedicated physical therapists and talented clinical team then design individualized treatment plans to achieve the specific goals for each patient per your doctor’s expectation.For More Information Call Now at: 301-498-1604
http://www.active-physicaltherapy.com/
 Genu Varum is defined as a lateral angulation of the knee. The longitudinal axis of femur and tibia deviates medially. The deformity involves tibia alone or the femur or tibia and fibula both.
Genu Varum is defined as a lateral angulation of the knee. The longitudinal axis of femur and tibia deviates medially. The deformity involves tibia alone or the femur or tibia and fibula both.