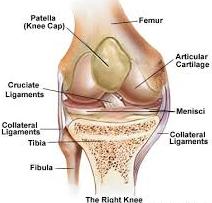
Causes and Treatment of Knee Injury:
Osteochondritis dissecans is a combined condition whereby a varying amount of cuboid and its nearby fibrous drops its blood flow. Osteochondritis dissecans can include the cuboid and fibrous of almost any combined. Joints are most commonly affected. In this condition, avascular necrosis occurs in an area of subchondral bone followed usually by degenerative changes in the overlying cartilage. Though it can occur in any joint, it is most commonly seen in the knee joint. This avascular bone undergoes necrosis, gets detached and forms a loose body. Infact, this is the most common cause for loose bodies within the knee.
Many causes are cited and are controversial:
- Exogenous trauma
- Endogenous trauma
- Ischemia
- Abnormal ossification within the epiphysis
- Genetics
- Combination of these
Common site
Lateral aspect of the medial femoral condyle near the attachment of posterior cruciate ligament.
Age groups
- In young patients before epiphyseal closure. Treatment outcome is good.
- In adults, here treatment outcome is poor.
Clinical Features
- It is different in the two age groups and consists of vague pain and discomfort in the knee, swelling, catching, popping and locking could occur.
- After complete separation, loose bodies can be palpated.
- Tenderness can be elicited over the anteromedial surface of the femoral condyle by deep palpation after flexing the knee.
Investigations
Plain X-rays of the knee (AP, lateral and tunnel view), arthroscopy, bone scan, MRI, etc. are some of the important investigation tools. Plain X-ray also helps to detect the loose bodies of the knee joints.
Treatment
- This depends on the age of the patient and degree of involvement.
- Treatment method varies from conservative in children to operative in adults.
- The operative methods are arthroscopic excision, curettage, pinning, debridement, grafting, etc.
- The outcome of the treatment is good in children and is not so good in adults.
If you are suffering from Knee Injury then contact today for Quick Appointment at Active Physical Therapy. Active Physical Therapy is the best Physical Therapy Clinic in Maryland.