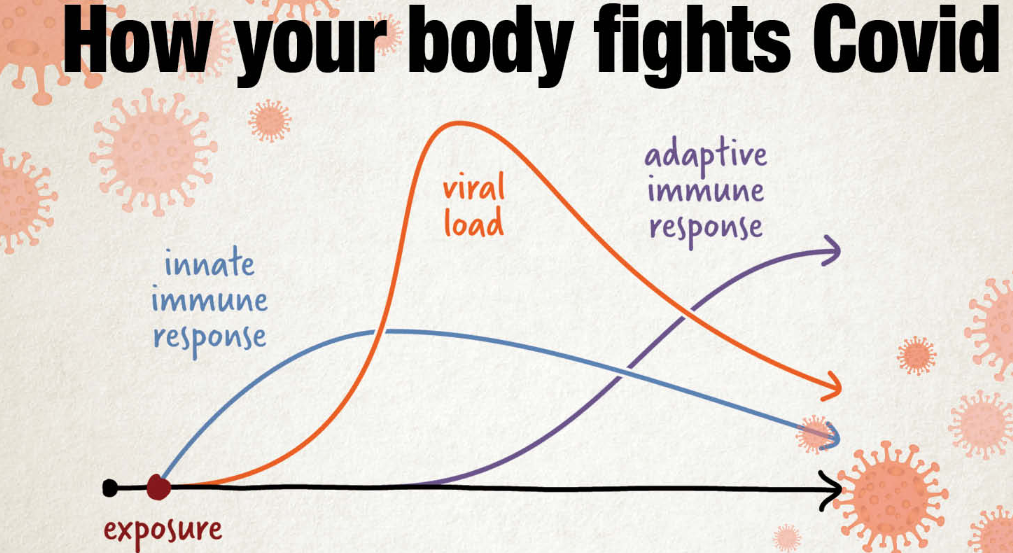
COVID -19 is a short name for the disease known as novel coronavirus 2019. Coronaviruses are a large group of similar viruses; some are known to infect humans. There are many different COVID -19 vaccines developed worldwide. You may be wondering how long after the second dose you have full immunity. The COVID -19 vaccine being so new and it studied so less, so questions are highly predictable. All the countries are still healing from the second wave of COVID -19 and undergoing strengthening of healthy immunity. Light fever and weakness are common after vaccines and these are normal to build immunity. First of all COVID -19 vaccines work depending on our body, that is how our body fights against illness. A strong immune system includes several tools to fight against infection. The vaccine contains inactive parts of particular antigens and newer vaccines contain the blueprint for producing antigens to oppose and fight the specific disease-causing virus. Inside the virus, genetic material called RNA is made up of genes, genes carry the information to make more copies of the virus. COVID -19 vaccine given with the needle triggers the immune response of the body. Influenza vaccines can trigger an immune response by mimicking viral infection. Vaccines are a product of science and train the body’s immune system to create a memory. When a pathogen again infects in the future, the body will rapidly prevent disease by remembering the threat. First Corona virus vaccine can prevent more than 90% of people from getting COVID -19; there are around a dozen vaccines in the final stages of testing.
Nations around the globe are racing to vaccinate people against the COVID - 19 virus. The scientific studies suggest that taking two doses of vaccine is significant for achieving the antibody response that provides overall protection and creates lasting immunity. The second dose activates the immune system much more quickly within a week of dose two. The second dose increases immunity tenfold and offers much stronger and long-lasting protection from the injection. COVID - 19 vaccines are safe and effective against severe disease and death from variants of the virus that causes COVID - 19. Two weeks after full vaccination like Pfizer and Modern vaccines are fully approved to protect, but after a single dose vaccine, you still need to follow the prevention methods such as wearing a mask and social distancing. COVID - 19 vaccines approved by WHO continue to be monitored to have a high efficacy rate of 50% or above. Immunity does not happen immediately after vaccination, because of this you can still become sick during this time frame.
Types of Immunity and Vaccines
Natural Immunity- Natural Immunity is the body’s actual immune response to produce antibodies against infection.
Vaccine-Induced Immunity- Vaccination starts producing antibodies to protect from diseases in the future.
Different Vaccines have different time periods to give a positive response.
· Pfizer- after Pfizer vaccine immunity starts developing about 12 days after the first jab.
Full immunity reached about 7 days after the second dose.
Pfizer is 92% effective after the first dose and 95% after the second dose. · Modern- Immunity starts developing from the 14th day after the first shot. Full immunity starts developing after 14 days of the second dose. The vaccine has an 80% efficacy rate after the first & 94% after the second dose. · Johnson & Johnson- Partial immunity starts developing after 2 weeks of shot. Full immunity develops after 28 days of the second shot.
Vaccines are 66% effective after full vaccination.
How Long Will Immunity Last?
Natural Immunity- Three types of white blood cells protect the immune system Macrophages, B- Cells, and T- Cells.
- Macrophages- Macrophages are white blood cells produced in bone- marrow, get matured and released into the bloodstream. The role of macrophages is to ingest and destroy bacteria, viruses, clean up debris and other harmful particles. That means macrophages will attack and break the viruses and bacteria when we are sick or shortly after the vaccine.
- B- Cells- B- Cells are key players in the body’s adaptive immune response. B Cells play a crucial role to produce antibodies that recognize unique parts of invading viruses, B- Cells fight bacteria and viruses. That means if the same infection gets into the body again, B- Cells will make unique antibodies and kill the infection right away.
- T- Cells- T- Cells have two types- Helper T- Cells and Killer T- Cells. T- Cells take care of B- Cells. T- Cells are slightly modified throughout the human lifetime. T Cells kill the damaged cells and the infection inside of them.
Vaccine-Induced Immunity- The same process after a vaccine is followed by the body to develop immunity. B- Cells, T- Cells, and Macrophages play the same role. Vaccines help the body to develop T- Cells and B- Cells that will remember how to fight the virus in the future.
Protection After Vaccine- Scientists have seen that vaccines will protect most people for the first few months after getting the second dose and no one really knows how long immune response and how many years from now COVID - 19. Vaccination has long-term protection and Key things to know about COVID - 19 vaccines.
Effectiveness- COVID - 19 vaccines are effective, they can keep you from getting and spreading the virus, you may resume many activities you did before the pandemic. Get vaccination regardless of whether you already have COVID - 19. For non- non-vaccinated communities, COVID is still a threat, even for those who did not have symptoms. Vaccines are not experimental but went through all required stages of clinical trials. Vaccines teach our immune system to recognize and fight the virus causes COVID - 19.
Mild – Reaction- after COVID -19 vaccination, you may have some side effects. The side effects from COVID - 19 vaccination such as tiredness, headache, or chills may affect your ability to do a daily activity but will go away in a few days. Vaccines are designed to give you immunity without the dangers of getting the disease. These mild effects after getting the vaccination signs that your body is building protection. Serious allergic reactions to the COVID -19 vaccines are rare. These minor symptoms usually happened after the second dose rather than the first.
Take Precautions- The far most essential precaution after taking the COVID vaccine is to continue wearing a mask after both doses. In fact, double mask protection Is still recommended. Vaccination allows you to stay unmasked, but it does not mean you should stop practicing precautions such as masking, social distancing, and hand hygiene.
Do & Don’ts after COVID - 19 Vaccination to Boost Immunity
1. Do’s –
- Drink plenty of water, and a hydrated body will reduce the symptoms you may face, preventing you from feeling sick.
- Eating a well-established diet such as green vegetables, turmeric, and garlic helps to boost immunity. Vitamin –C-rich fruits also fight the vaccine side effects.
- In case a person has allergies to medication or drugs, it is important to get an all-clear from medical practitioners such as people on steroids and diabetes.
- Vaccinated lactating mothers should continue breastfeeding as babies can get through milk.
2. Don’ts-
- Don’t be afraid after vaccination, some feel unpleasant, dizzy, and feel strong pain. Don’t worry about the post-effects of Vaccination. These effects give signs that your body is naturally reacting to the vaccine.
- It all depends on your body to handle the effects of the vaccine. Your body needs to rest as much as possible. Don’t do such strenuous activities within the first 24 hours. Start light exercise after 24 hours of the COVID vaccine.
- Do not consume alcohol or smoke, Avoid tobacco also. Alcohol affects the body’s immune system negatively and there is a chance that the immune response to the vaccine may not be as effective.
- Do not miss other necessary vaccines, and do not stop taking precautions. A person could still get infected by COVID -19 in a few days immediately following the vaccination because the person would not have had enough time to develop immunity.
Contact Active Physical Therapy
 Biceps Tendinitis
Biceps Tendinitis Your hands help you in cooking, cleaning, brushing, typing and in every type of daily routine activities that you perform. But you do not notice the importance of hands unless some impairment or deformity makes it difficult for you to use your hands.
Your hands help you in cooking, cleaning, brushing, typing and in every type of daily routine activities that you perform. But you do not notice the importance of hands unless some impairment or deformity makes it difficult for you to use your hands. 



